Ever wondered how to make better use of evidence in decision-making? Follow our latest blog series to find out more about how our Evidence and Knowledge Mobilisation team can help you to make sense of and use evidence from research and practice.
We’ll share with you some ideas for how our work can help you to adopt digital health innovations, even when evidence seems limited.
And if you’ve ever wondered just how we find our way through all the evidence out there, this is a great opportunity to learn more about how we’re testing out new and innovative ways of working to manage and share our work.
And later in the series, we’ll share with you why knowledge equity is so important for addressing health inequalities.
For Part 1, we’re going a little bit abstract! Alison sets the scene, describing our approach to what we do.
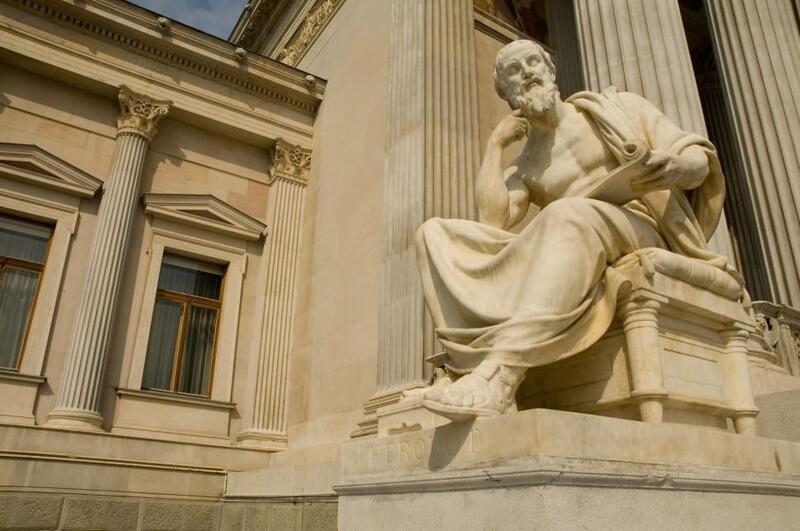
What’s philosophy got to do with evidence reviews?
Research and innovation are important drivers for improvement in health and care. But we often struggle to make the best use of what we learn from testing out ideas. Interventions or innovations which seemed promising don’t always translate well to other settings. Philosophy can help us to understand why that might be.
How we learn and test out new ideas is influenced by how we make sense of the world around us. At the risk of (massive) oversimplification, let’s consider two contrasting views.
First, meet Sam, a researcher who specialises in randomised controlled trials (RCTs). (If you’re familiar with the evidence-based medicine (EBM) movement, you’ll remember the evidence hierarchy, featuring RCTs as the gold standard method for measuring effectiveness with some calling for wider adoption in public policy).
Sam believes their role as a researcher is to observe and measure what is happening, drawing out generalisable facts. Sam sees themselves as a neutral observer and uses methods (like randomisation and blinding) which control for bias. Sam aims to be objective, making sure their methods can be replicated and their findings can be generalised.
Now meet Andi, who has a different way of understanding the world. Andi recognises that our experiences of health and care will be different – our environment affects what we can access and our experiences shape how we behave.
Andi believes their role as a researcher is to understand the world from different perspectives. So, they explore values, attitudes, thoughts, experiences and behaviours.
Andi is interested in understanding how or why an intervention or innovation works (or doesn’t!) in a specific context.
Obviously, it’s a lot more nuanced than I’ve described here, but the key point is that there are different ways of looking at and understanding health and care and the impacts on people.
Why does this matter?
Our view of the world can mean we prefer to use certain types or forms of knowledge to make decisions. And this can lead to gaps in our understanding.
Because health and care is so complex, it’s important to be aware of such gaps. For any improvement we try to make – for example, a new service, a new way of working or a new technology – people and communities will respond in different ways and there will be consequences we don’t expect. Blind spots are inevitable but by looking at problems from different views, we can build a fuller picture.
Ultimately, our role in the Evidence and Knowledge Mobilisation team is to make sense of evidence from research and innovation within this complex environment.
Our approach is to review multiple sources and types of evidence from a range of disciplines. Evidence from Sam’s research can help us to reliably understand the potential value of an intervention or innovation, its benefits and harms. But we also use Andi’s research to understand the complexity. For example, the potential impacts at an individual or community level and the human, social and organisational factors involved in implementation.
If we had to describe our way of looking at the world, we’d opt for pragmatism. We find the evidence hierarchy doesn’t really work for most of the questions we’re asked to consider. Our approach is more “horses for courses”, focusing on the types and sources of evidence most appropriate for the type of question.
Every day, research discoveries and service innovations identify potential for improvement in health and care. By navigating this complex evidence landscape and translating findings into useable insights, we aim to help our health and care colleagues to realise that potential.
Coming soon...
- What does it mean for an ICS to be evidence-informed?