“Champion, challenge, collaborate.”
Being commissioned by the Mayor of London to produce independent reviews of proposals for major service change, affecting Londoners, perfectly aligns with our commitment to help the health and care system make better decisions and ultimately achieve benefits for population health and wellbeing.

Our role in the New Hospitals Programme
Learn how the Strategy Unit’s innovative model is transforming hospital planning by providing a consistent, data-driven approach to forecast future demand and evidence-based decision making.
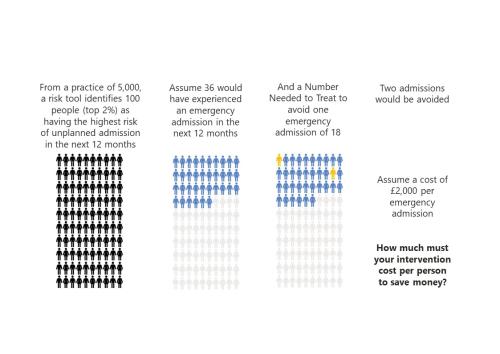
‘To risk stratify or not risk stratify, that is the question’ (At least, it should be)
Risk stratification tools are ubiquitous in healthcare. The concept is simple and seductive.
Contracting for health outcomes: from concept through theory to implementation
In this new report, jointly authored with colleagues from the University of York and The Royal Orthopaedic Hospital NHS Foundation Trust, we set out in detail how an outcomes-based contract for elective knee replacements might be constructed, and the potential implications for commissioners, providers, and policy-makers.
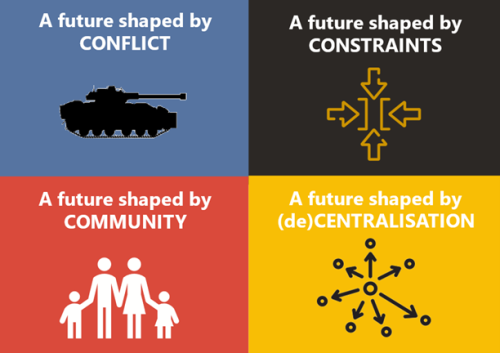
Exploring the Edge of Tomorrow, Today
Exploring the critical building blocks for a resilient social care system in 2035 with the West Midlands Association of Directors of Adult Social Services (WM-ADASS).
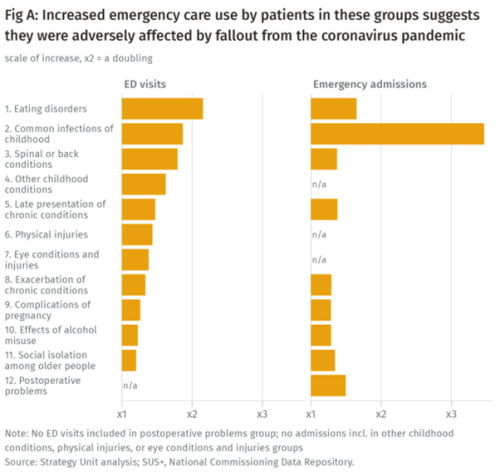
Population health implications of the Covid-19 pandemic
Our new report for The Midlands Decision Support Network (MDSN) presents findings of the effects of the care disruption, from the Covid-19 pandemic, on population health. The in-depth analysis identifies which patients and health conditions should be the focus of future efforts in reducing inequalities caused by the pandemic.

What are the ethical challenges in addressing inequities?
Produced by Angie Hobbs - the world’s first Professor in the Public Understanding of Philosophy – this paper examines the ethical questions raised by our report outlining strategies for reducing inequity.

Helping ICSs to reduce inequalities in access to planned care
Are there inequalities in access to planned care? If so, what are they? Which groups ‘gain’ and which groups suffer? And what could be done to address any inequalities? In pursuing their objective of reducing inequalities, what could Integrated Care Systems (ICSs) do? What strategies and approaches are likely to be successful?

Blog: Strategies to reduce inequalities in planned care
MDSN responds to recent reports addressing the NHS waiting list crisis

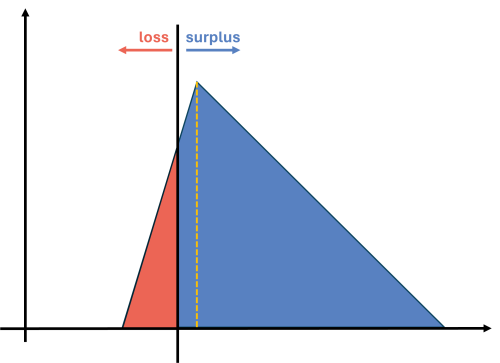
‘Might’ is right
A good idea can be ruined by over-selling.

Strategies to reduce inequalities in access to planned hospital procedures
UPDATE 10th August: Now including briefing note for Integrated Care Boards on legal duties in respect of reducing inequalities. This report guides ICBs through the process.

Appointing an ICS ‘Chief Analyst’
The Strategy Unit has, over the last ten years, developed a way of working that has allowed us to become recognised as a leading analytical organisation in the NHS.

Treating people on waiting lists: who decides what is fair?
Waiting lists for elective care are in the news. The national plan has been issued, with the expectation that lists will continue to rise for some years - and that long waiting will not disappear anytime soon. Addressing this ‘backlog’ will remain a fundamental challenge for some time to come.

Decision makers can make much better use of analysis
Part of the Strategy Unit mission is to improve the use of analysis in decision making. Current use is, to employ a euphemism, variable.

Advancing the analytical capability of the NHS and its ICS partners
The Strategy Unit were asked by the Strategy and Development Team in the Directorate of the Chief Data and Analytics Officer, NHSE/I, to make recommendations for advancing analytical capability across the health and care workforce.
INSIGHT 2021: Insight to action - lessons from think tanks
The Midlands Decision Support Network exists to support health and care leaders generate insights from high quality analysis and evalu

Strategy Unit devises a new method for classifying outpatient appointments
The number of outpatient attendances in England is now approaching 100 million each year.

INSIGHT 2021: The most valuable value - a health and care resourcing dilemma
We heard discussions from experts from the NHS, NICE and academia (Andi Orlowski, Gwyn Bevan, Deborah O’